Keratoconus
At the Amigó Ophthalmological Institute we are achieving improved vision quality, reducing or eliminating dependence on glasses and contact lenses.
| Keratoconus is a progressive deformation of the cornea that in its final stages takes on
a conical shape, which progressively alters the quality of vision.
Unfortunately keratoconus is usually difficult to identify early on without special equipment and expertise in early diagnosis. Therefore, at the Amigó eye clinic we use not one, but several different corneal topographers (Pentacam, Keratograph), wavefront aberrometers (Ladar Wave) and equipment specialised to detect subtle degrees of corneal weakness (ORA). When the disease is not too advanced, patients can wear glasses. But when it progresses further, it cannot be adequately corrected with glasses and they complain of never managing to see well with them. In these cases rigid contact lenses are used, which although they improve vision, do not stop the progression of the conical malformation. keratoconus surgery is the only way to stop the progressive deformation of the cornea and successfully improve vision in many cases. |
There are various techniques for this:
|
Keratoconus Surgery
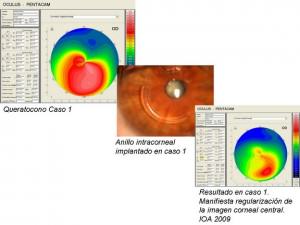
This hereditary disease of the cornea is highly prevalent in the Canary Islands. Until now, people suffering from it were excluded from surgery aimed to improve the defective vision it causes. The new techniques of intracorneal ring implantation and corneal cross-linking that are currently performed at the IOA have enabled us to improve quality of vision in its sufferers, reducing if not eliminating their dependence on glasses or contact lenses.
Even corneal transplants, previously the only option in advanced cases, may thus be avoided. The IOA has the most advanced equipment for corneal tomography (Pentacam), for diagnosis, and later monitoring of patients once intracorneal rings are implanted.
1. What is keratoconus ?The cornea is the transparent front wall of the eye which acts as a natural lens. Keratoconus is a disease that alters the normal shape of the cornea, causing a progressive deformation which in the final phases takes on a cone shape. This gradually alters the visual quality of the affected eye. 2. What causes keratoconus ?It is clearly a hereditary disease but with ‘variable penetrance’, that is it can affect minimally or even to a severely advanced extent, ranging in intensity not only between patients but between the pair of eyes (it occurs bilaterally and asymmetrically). This process depends on the age of the patient and when the symptoms start to appear. Usually the younger the patient and the earlier the onset of keratoconus, the faster the progression, and its early diagnosis strongly influences the success of treatment. |
3. How is keratoconus detected ?In more advanced cases detection is simple. Unfortunately most initial keratoconi are difficult to diagnose without special equipment and experience in early diagnosis. Therefore, the Amigó Eye Institute uses not just one but several different corneal topographs (Pentacam, Keratograph), wavefront aberrometers (Ladar Wave) and specialised equipment to detect subtle degrees of corneal weakness (ORA). Together with our extensive experience in the early diagnosis of keratoconus, these aids not only permit us to diagnose keratoconus in the early stages but also the less obvious “forme fruste”, almost undetectable by other methods. Their timely identification often positively influences the final visual outcome. |
|
|
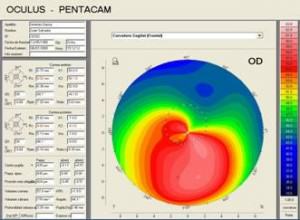
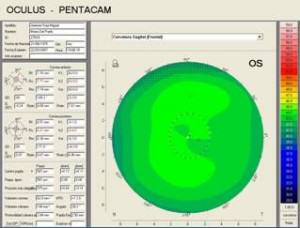
On the right you see two corneal topography images for the diagnosis of
keratoconus. The shades of green in the top image correspond to a normal cornea. In the
lower image, intense reds indicate the presence of keratoconus. Case 1. |
||
4. How is keratoconus operated on?When the disease is not too advanced, patients can wear glasses. But when it progresses, it cannot be adequately corrected with glasses and they complain that they never manage to see well with them. In these cases, rigid contact lenses are used that, although they improve vision, do not stop the progression of the conical malformation. Keratoconus surgery is the only way to stop the progressive deformation of the cornea and in many cases successfully improve vision. How is keratoconus operated on?Keratoconus is thus a malformation of the cornea which affects vision. It can be progressive or halt at a certain age, with greater or lesser impact on vision. Consequently, the treatment also varies whether the degree of visual impairment is advancing or not. |
|
Here we answer some of the frequently asked questions about the two treatments performed at the Amigó clinic: cross-linking and intracorneal rings.
CROSS LINKING[wpspoiler name=”What is it and how is it achieved?”] Cross-linking involves the application of a hardening substance (Riboflavin – vitamin B2) onto the cornea while illuminated with ultraviolet light, to achieve increased cross-linking of the collagen fibrils that make up the corneal tissue. This holds corneal deformation at bay and can improve visual quality.It is a painless technique only requiring anaesthetic drops to numb the eye surface. The patient lies down looking towards a light source while Riboflavin is dripped on the affected eye. Treatment is not short, in total it lasts just over an hour. [/wpspoiler][wpspoiler name=”What is the result in terms of vision?”] Stopping this disease and its progressive worsening of vision is a real and up to now unthinkable success of this surgery.We must clarify that the visual recovery after treatment may take several months, but this is often accompanied by an improvement in the quality of vision of the operated eye. [/wpspoiler][wpspoiler name=”What are the risks ?”] There are risks inherent in any surgical technique. Due to the fact that cross-linking acts directly on the corneal surface, delay or disturbance in healing can occasionally occur, resulting in a slower visual recovery.[/wpspoiler] |
INTRACORNEAL RINGS[wpspoiler name=”How is it done and what are they made of? (Keraring, Intacs)”] It is a surgical treatment that respects the cornea, without penetrating inside the eye like a corneal transplant does. One or two rigid semicircular segments are implanted within the cornea, which act to tighten and regularize the centre of it, thus improving quality of vision.The rings are made of Perspex, an acrylic material used for over 25 years in the manufacture of intraocular lenses. It has proved to be perfectly tolerated by the body, without the risk of rejection. Such surgical treatment with intracorneal rings is far safer and less traumatic for the correction of keratoconus than corneal grafts, provided deformation is not overly advanced. [/wpspoiler][wpspoiler name=”What is the surgical technique like?”]At the Amigó eye clinic the entire procedure is performed under a surgical microscope with topical anaesthesic to avoid any pain, i.e. drops only, without any injection. The procedure lasts between 10 and 15 minutes and the next day the patient may perform basic activity while treatment with eye drops is maintained for a few weeks. [/wpspoiler][wpspoiler name=”What are the risks ?”] The risks are minimal. One of the main advantages is the reversibility of the ring. In rare cases with signs of infection or incorrect healing the ring can be removed, returning the cornea to the state prior to the operation.[/wpspoiler][wpspoiler name=”What are the visual results?”] The degree of improvement depends on the extent of progression of the keratoconus, since patients operated on in the early stages benefit most from surgery, with an exceedingly high success rate (85-90 %). Visual recovery is rapid and usually already noted from the first few days on, but it should be remembered that the use of glasses or contact lenses may be necessary to complete the visual improvement.
Today surgery with cross-linking and/or intracorneal rings is our
technique of choice for the surgical treatment of keratoconus, given the rapid recovery and
scarce complications.
|
Back to
|
Learn more aspects ofof keratoconus on our blog.